Mealtime Partners, Inc.
Specializing in Assistive Dining and Drinking Equipment
February 2011 Independent Eating and Drinking Newsletter
 |
February Topics: |
||
|
Mealtime
Partners Home Page Send a Comment or Suggestion |
|||
The High Cost of Under Nourishment
The American Dietetic Association (ADA), in compiling a position statement on the cost effectiveness of medical nutrition has shown that it is far less costly to maintain good nutrition levels than to cover the medical costs that result from illness that occur in people who are under or malnourished. For every dollar spent on nutrition services, at least $3.25 is saved in medical costs. Malnutrition leads to a higher incidence of acute illnesses and infections than occur in individuals who are well nourished. Also, the incidence of complications during an illness is four times greater in individuals who are under or malnourished and reoccurrence of illness occurs more frequently than in well nourished individuals. The medical treatment and recovery time for malnourished people is on average one third longer than for those who well nourished, and additional days spent in the hospital equates to higher medical costs.
Under or malnutrition has many causes. However, most people in the United States believe that it is only present in under developed countries. In the United States there are several groups who are seriously impacted by under nutrition. The first group is people whose economic status does not let them buy adequate food. Other groups typically have health problems that are responsible for under nutrition. In many cases these people are unable to eat without difficulty because they have oral motor difficulties, and/or swallowing problems, or problems with their digestive system. A small group of children do not have an adequate awareness of hunger, or are resistant to eating. This particular group of children needs special treatment from a feeding specialist or a feeding clinic.
For those who are unable to consume enough calories by mouth to sustain growth and health because of eating difficulties, tube feeding is sometimes considered as assistance or a substitute for oral eating. Another approach to increasing the value of the food that is consumed is boosting its caloric and nutritional content. A doctor and/or dietitian should guide the diet changes that boost calorie intake. The type of calories used to increase calorie count per ounce can vary significantly and can be calories from protein, carbohydrates, or fats. Calorie boosting can be done using regular table foods like butter, cream, olive oil, or over the counter or prescription additives that can be either a powder or liquid. In either case they are added to a regular diet to maximize calorie intake per bite.
A large group of people who have difficulties with maintaining good nutrition are the elderly. Once again there are many contributing factors to their decline in nutritional intake. Some factors, like loss of taste relate to the aging process (refer to the second article in this Newsletter for more about taste); other factors, like arthritis, relate to the actual mechanism of preparing and eating food. As people age and develop disabilities and illness, they become more and more dependent for care. One program that helps elderly people remain in their homes and eat well is “Meals On Wheels” (www.mealsonwheels.org) who deliver meals to many homebound people. However, many elderly people require a significant level of nursing care and become residents of nursing homes.
Unfortunately, not all nursing homes are created equal and a high rate of malnutrition and dehydration1 exists in nursing homes through the United States. When individuals move to a nursing home many are already in need of help at mealtimes. The U.S. Census Bureau estimates that 21% of nursing home residents must be fed, while 26% need help at mealtimes. The Nutrition Screen Initiative estimated that 40% of nursing home residents are under nourished. Greene Burger, et al,1 identified inadequate staffing as being responsible for the high incidence of under nutrition in nursing home residents. The Nursing Home Abuse Resource Center estimates that it takes 30 to 60 minutes to feed a person safely and sufficiently, but that nurses’ aides may be assigned to feed as many as 15 people at each meal. This results in people being fed too quickly, or forcefully, or receiving an inadequate amount of food.
Long-term care services in the United States cost over $180 billion in 2002 and still we have an epidemic of malnutrition and dehydration going on in nursing homes throughout the U.S. The delivery of home and community based services have been shown in studies2, 3 to be a cost effective alternative to nursing homes. Also, the vast majority of Americans would prefer to live in the community not a nursing home, yet this option is not always available due to budget constraints and long waiting lists for community based services.
With the vast expense of caring for the disabled of all ages, different strategies need to be tested for providing adequate nutrition to both those who reside in their own homes and nursing home residents. Schools are already embracing the use of assistive technology for a broad range of applications from communication devices, and computers that can both read and write text, to dining equipment. For the elderly, a progressive nursing home could provide Mealtime Partner Dining Systems to those residents who need to be fed and who would be comfortable using assistive technology. With the expansion of the use of computers and smart phones it is not surprising to see how many older individuals enjoy email, Facebook, and other “aps” on their cell phones. For those people, to feed themselves using technology, rather than being fed might be a far better experience. Regardless, as the baby boomers age and become disabled, the numbers of elders who will require care is going to escalate and overwhelm the already understaffed nursing homes. Technology, by necessity, will become more common-place and will be invaluable for maintaining nutrition and well being.
| Did You Know? Did you know that Mealtime
Partners, Inc. makes custom drinking systems
for those individuals who are unable to find an over-the-counter
drinking system to meet their unique needs? De-hydration is an
ongoing problem for many people, especially
those with disabilities. It is responsible for health problems
such as urinary tract infections, kidney problems, skin tissue
deterioration, and headaches. All of these conditions require
medical treatment that, in some cases, can be protracted,
require hospitalization, and thus be very expensive. For complete information on all of our currently available drinking systems click here. If you don't find a drinking system that meets your personal needs, email: drinking@mealtimepartners.com, or call us at (800) 996-8607 for more information about a custom drinking system. We can assist you in deciding which system is most appropriate for your client or family member, or in developing a custom drinking system. Preventing dehydration is a cost-effective method for reducing long term health costs. |
An Update on Our Ability to Taste
This article is an update on information relating to how we taste. Many prior Newsletters that Mealtime Partners, Inc. has published have discussed the issue of our ability, or lack of ability, to taste various foods. In particular, the January 2010 Newsletter discussed the importance of Food Flavor. The flavor of food is important to its enjoyment. If you have reduced sensitivity to taste, stronger flavor is necessary to be aware of food having any flavor. Individuals do not appreciate subtle flavors if they have reduced sensitivity of their taste buds. One of the byproducts of loss of taste is loss of desire to eat. This puts individuals at a risk of undernutrition or even, over time, malnutrition.
The roof of our mouth and tongue are covered with thousands of taste buds that provide us with our sense of taste. When we eat, the taste buds send messages, through sensory nerves, to the brain and thus we are aware of different flavors. The picture (shown below) illustrates how it is commonly believed that we taste things with our tongue. This belief has been well established for many years and the illustration has been published in text books as an accepted standard.
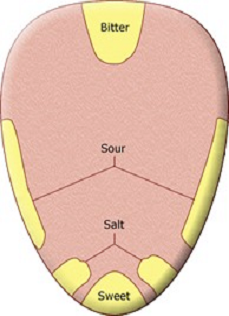
However, this information is false. It has come from an English mistranslation of a German research paper4,5 and has been scientifically disproved by later research. Yet it has continued to be printed in textbooks for almost 100 years. The misunderstanding originates in the translation of, “showed minute differences in threshold detection levels across the tongue”. This statement evolved into “as a difference in sensitivity” and thus the myth began.
As a result, to the original basic tastes: bitter, sour, salty, and sweet, a fifth flavor should be added: umami. In common terms, umami can be described as a savory taste that can be found in soy sauce, tomatoes, oysters and other foods that are high in glutamate. Umami is a word that comes from the Japanese and means “flavor” or “taste”.
It is now understood that any part of the tongue can pick up any taste, but sensitivity varies across the tongue. The tongue is covered with bumps that have been described as taste buds. They are actually fungiform papillae and each of these bumps that are like tiny mushrooms, or barrels, contains 50 to 100 taste buds (also called gustatory calyculi). There are far more taste buds that sense bitter than any other flavor. It is thought that this is the body’s way of protecting itself from being poisoned. Many toxic materials and poisonous plants are extremely bitter.
Not everyone has the same number of taste buds or have taste buds that are equally sensitive. Though most taste receptors are found on the surface of the tongue there are some in the throat and soft palate at the back of the mouth. The ability to taste begins before birth and babies seem to respond favorably to flavors that they were exposed to in the womb. They also respond well to flavors that they taste through breast milk. Our original taste preferences stem from the genes inherited from our parents but, as we grow and are exposed to our environment, we learn to enjoy new tastes.
Our taste buds have help with sensing taste from our nose. Olfactory receptors inside the upper part of the nose are able to sense smell and send massages to the brain about the smell. This information, along with the information that is being sent to the brain from the taste buds, provides a broad view of the true taste of what is being eaten. When someone has a cold or allergies, they frequently find that food does not taste the same. This is explained by the missing information from the olfactory receptors.
Regardless of how well we taste and our personal food preferences, the flavor of food should provide pleasure to the person eating, otherwise mealtimes are dull and the result can be that the person does not eat well and might lose weight, thus compromising their health. After an illness, it is common for the taste buds to be impacted and care should be taken with the food being served to make it as appealing as possible.
|
Independent Drinking Medical treatment for rehydration is estimated to have exceeded $1 billion in the U.S. in 1999 for elderly patients, alone6. For most individuals, dehydration is 100% preventable, yet many people with disabilities suffer from some level of dehydration almost constantly. The Front Mounted Drinking System provides hands free drinking throughout the day for those who sit in a wheelchair and are unable to lift or hold a cup or glass, and is designed especially for those who have weak suction and cannot use a Drink-Aide or Hydration Backpack.The Front Mounted Drinking System is quick and easy to mount. The liquid container fits into a drink holder that is positioned near the mouth of the user by bending the appropriate length "gooseneck" support arm. The drinking tube is semi-rigid and can be positioned near the lips of the user. The drinking tube is much shorter than any other hands-free drinking system, allowing use by individuals with a reduced ability to produce a suction. Making liquid always available allows the user to drink whenever they want. This lowers the risk of dehydration and improves the quality of life for those who use this system. |
The Front Mounted Drinking System The Front Mounted Drinking System comes with wheelchair clamp, a heavy-duty gooseneck support arm (four lengths are available), cup holder with clamp, and a koozie. The cup holder can accommodate a variety of (user provided) cups and bottles. A koozie is provided to keep drinks hot or cold. This is the easiest to clean of all Mealtime Partners drinking systems because disposable straws can be used and there is no long drink tube to clean. |
| For more information about all Mealtime Partners drinking systems and information about choosing the most appropriate drink system, click here. | Click the following link for prices and/or for ordering the Mealtime Partners Front Mounted Drinking System. |
| The Front Mounted Drinking System is only available from Mealtime Partners, Inc. | |
February 2011 Newsletter References:
1. S. Greene Burger, J. Kayser-Jones, J. Prince Bell. Malnutrition and Dehydration in Nursing Homes: Key Issues in Prevention and Treatment. National Citizens’ Coalition for Nursing Home Reform, July 2000.
2. Kassner, E. Medicaid and Long-Term Service and Supports for Older People: Fact Sheet. Washington, DC: AARP Public Policy Institute, 2005.
3. Miller, N. A., Harrington, C., Goldstein, E. 2002. Access to community-based long-term care: Medicaid’s role. Journal of Aging and Health Volume 14, No. 1: 138-59.
4. Hanig, D.P.,1901 Zur Psychophysik des Geschmackssinnes. Philosiophische Studien, 17:576-623.
5. Pelletier, C. (2002). Beyond the Tongue Map: Evaluating Taste and Smell Perception. The ASHA Leader.
6. Pershad J. A systematic data review of the cost of rehydration therapy. Applied Health Economics and Health Policy. 2010; 8(3): 203-14.
Mealtime Partners Website Navigation:
Home | Dining | Drinking | Videos | Products | Warranty | Ordering | Calendar | FAQ | Newsletters | Contact
Please send comments and suggestions to newsletters@mealtimepartners.com
Copyright © Mealtime Partners, Inc. 2011
All rights reserved.
